- Patient Information
- Making an Appointment
- Having an operation? What to Expect
- Post Operative Review
- Shoulder Imaging
- Steroid Injections
- Driving after my surgery
- Wound care
- Patient Booklets
Making an Appointment
If you are a new patient and wish to make an appointment, please send a referral from your GP or Physio, along with any written reports of scans you may have had done on your shoulder. Once the referral has been received and triaged, a member of the team will contact you.
If you are an existing patient you can call us or send an email with your query, please include your date of birth on the email.
Email: hannanmullett@upmc.ie
Making an Appointment
If you are a new patient and wish to make an appointment, please send a referral from your GP or Physio, along with any written reports of scans you may have had done on your shoulder. Once the referral has been received and triaged, a member of the team will contact you.
If you are an existing patient you can call us or send an email with your query, please include your date of birth on the email.
Email: hannanmullett@upmc.ie
Having an operation? What to Expect
Prior to the date for your surgery you will be provided with an information leaflet and guidelines as to your arrival time at the hospital and a fasting guide.
Usually, you need to fast for 6 hours prior to a General Anaesthetic. For a local anaesthetic or injection procedure you do not need to fast.
You will also likely meet the anaesthetist who will put you to sleep and the physiotherapist will discuss the rehab plan with you. You will have the surgery explained again to you and you will need to sign a consent form. A mark will be placed on the correct side for the surgery, don’t worry though these are all routine protocols and procedures for all surgery in Ireland.
You will be asked to change into a surgical gown. For shoulder surgery it is unnecessary to change into the surgical undergarments and you may wear your own under the gown, but please remove your bra if you are wearing one. From here you will be brought into the theatre anaesthetic room to be put to sleep.
It is important to note that you are legally not allowed to drive for 24 hours following a general anaesthetic, so you will need a delegated person to bring you safely home.
For Day case procedures you can usually be discharged home 4 hours after your surgery. That said, if you are unwell, have not been able to tolerate oral fluids, food or passed urine we keep you overnight to ensure the anaesthetic has worn off. For the more invasive surgeries, an overnight stay is usually required, so bring night clothes, toiletries, dressing gown and slippers. At the time of booking the surgery we will inform you if we are planning you as an overnight case or Day surgery.
After surgery you will have limited use of your operated arm, this is usually in a sling and can be rather sore, but you should be able to manage self-care with the other arm. Not all slings are created equal and some may require you being taught by the physiotherapists how to properly put the sling on and off. Don’t worry this will all be done prior to your discharge. The length of time you will need the sling for with likewise vary on the operation, so myself or a team member will explain that to you after the operation.

During the operation you will have been given 2 doses of local anaesthetic to reduce the post-operative impact of pain. These injections last anywhere between 6-8 hours. Ideally you should be relatively comfortable when you wake up, however once the local anaesthetic wears off you may get a ‘rebound’ of pain, and we would advise taking the prescribed pain medication from the anaethetist.
You may be asked by the nurse looking after you to take some pain medication prior to the local anaesthetic wearing off, this is to reduce the severity of the rebound when it does occur. By adequately managing this rebound phenomenon early, patients often have less pain later, require less heavy-duty pain killers overall and rehabilitate faster.
Post-Operative Review
Following surgery an appointment will be made for you to see our Clinical Specialist Physiotherapist, Ms Clare Gilsenan or Ms Michelle Clarke.
At this appointment, Clare or Michelle will explain what Mr Mullett found and the procedures he performed during your operation. They will advise on what to expect in the coming 6 to 8 weeks in terms of pain and shoulder function. They will review your wound to check it is healing.
Physiotherapy is very important to optimise the results of your surgery. You will be given a referral and protocol to attend your local physiotherapist.
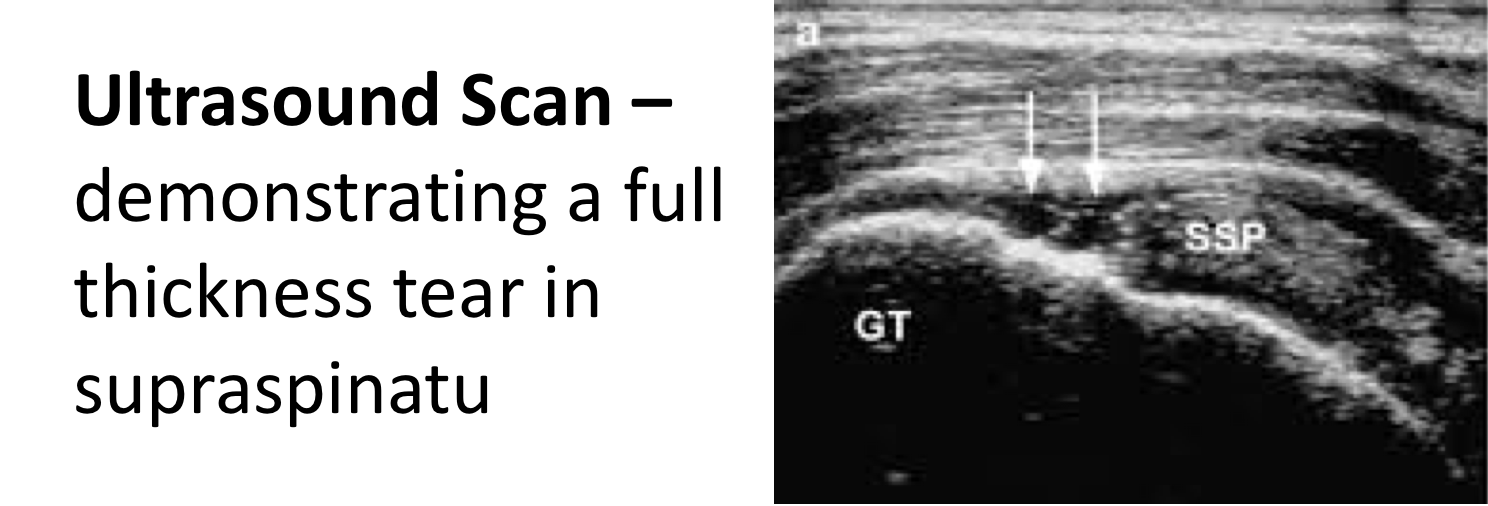
Shoulder Imaging
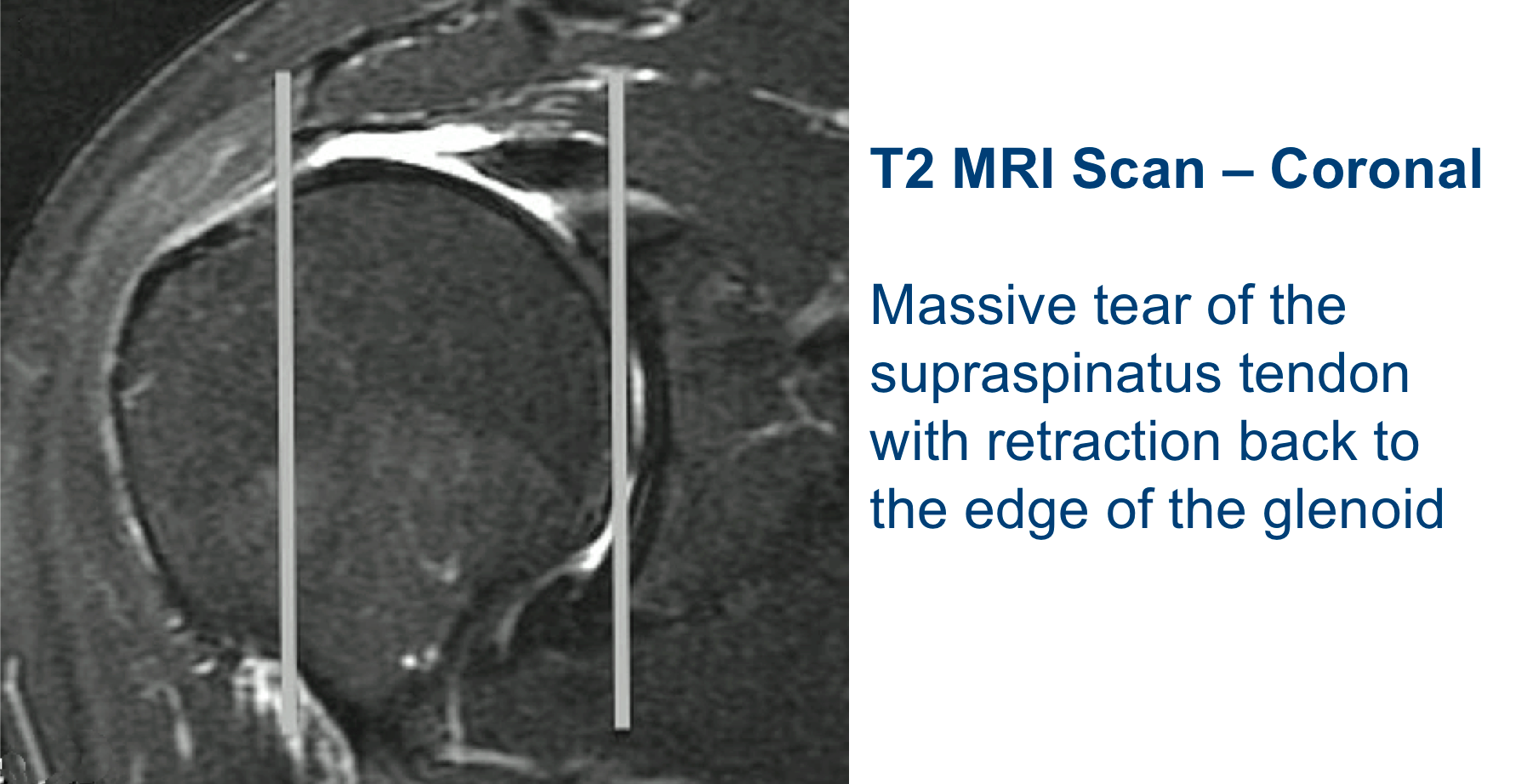
We as clinicians often use different type of medical imaging to assess differing structures in the body. This is no different in case of the shoulder. It may be that you have one form of imaging done at the time of referral but due to your injury/needs further imaging it required. At the point of consultation, our team will let you know if this is the case.
X-Ray: good for bone position and composition. Used to assess shoulder position in a case of disloactioin/relocation, fracture or in the case of shoulder arthritis.
Ultrasound: not as commonly used but still good for soft tissue injury; rotator cuff tears, tendonitis and condition of the caspular lining of the joint.
MRI: current gold standard for assessing the ligaments, tendons, muscles and bone structures of the shoulder.
MR-arthrogram: this is similar to an MRI but it uses a dye injected into the shoulder joint to give further detail on the stability of the shoulder joint itself, often used in instability/dislocation cases. This scan is done awake.
On the day of consultation:
If you have already had imaging of your shoulder please either bring scans (on disc) unless they are also available online e.g. Affidea.
The radiology report may have been sent to us which is helpful but we will need to review the images also. If Plain xrays are necessary they can be performed prior to the consultation by arrangement – Gráinne or Orla can arrange them. If we feel that you would need a Xray or MRI prior to first consultation one of our team will contact you to arrange it prior to consultation.
If you have already had imaging of your shoulder please either bring scans (on disc) unless they are also available online e.g. Affidea.
The radiology report may have been sent to us which is helpful but we will need to review the images also. If Plain xrays are necessary they can be performed prior to the consultation by arrangement – Gráinne or Orla can arrange them. If we feel that you would need a Xray or MRI prior to first consultation one of our team will contact you to arrange it prior to consultation.
Steroid Injections
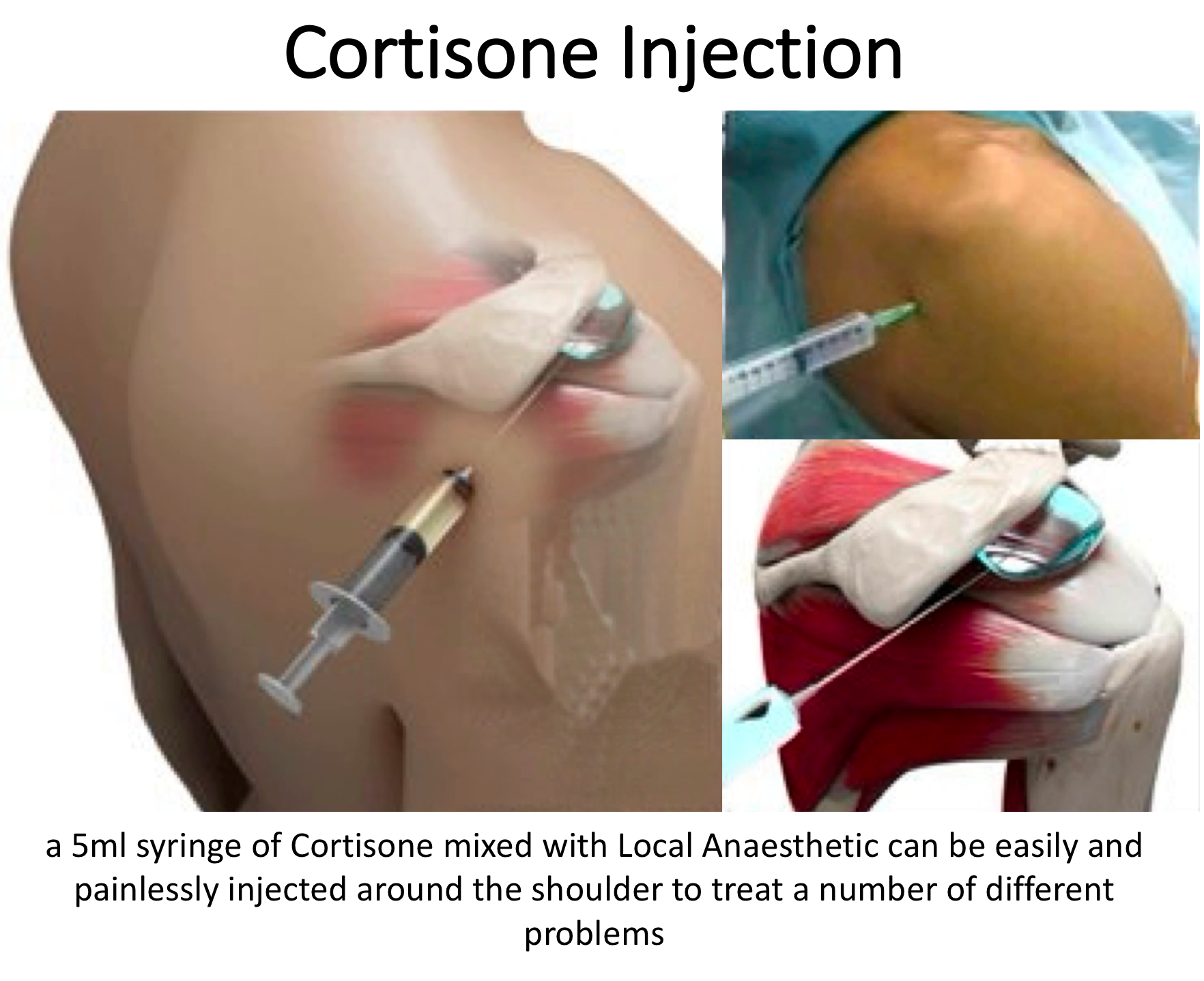
Cortisone is a potent anti-inflammatory medication that is a type of steroid.
Cortisone injections make up a very important part of the treatment of shoulder injuries. In combination with an active rehabilitation program they may significantly reduce the need for surgery in shoulder impingement syndrome.
Cortisone injections are useful in the treatment of various musculoskeletal conditions, particularly those of acute inflammation (such as acute bursitis), and degenerative joint and tendon conditions.
It may be suitable that at the time of consultation, you are given a steroid injection so please do not be surprised by this. This will be decided usually following a thorough discussion and examination.
In the shoulder injections are particularly useful in the management of:
- Rotator cuff disease (degenerative tendonosis, impingement, partial tears and subacromial bursitis)
- Adhesive capsulitis (or ‘frozen shoulder’)
- Glenohumeral osteoarthritis
- Acromioclavicular joint disease (osteoarthritis or osteolysis) Local cortisone injections may cause some side-effects. These would include:
- Systemic absorption. Care should be taken in diabetics as blood sugar levels may rise
- Infection – The medical literature suggests this occurs in less than 1:20,000 cases. It can be avoided by using a sterile ‘no touch’ technique with the needle and an alcohol swab
- Crystal flare – As previously mentioned occurs in 1:20 patients and can be treated with ice and paracetamol
- Skin changes – Skin atrophy & pigment loss may occur around the injection site. This is generally a minor cosmetic problem and occurs in less than 1:100 patients
- Bleeding (especially if patient has a bleeding tendency)
Driving after my surgery

The time taken before someone can return to driving after shoulder surgery will depend on the type of procedure undertaken, the length of immobilisation (if required) and the recovery of active movements. To be able to drive safely you should be capable of actively moving your shoulder without assistance and without damaging the surgical repair. You should be able to react normally to avoid causing injury to yourself or others due to lack of control.
- It is a requirement that, unless specific dispensation has been granted by the DVLA, a driver uses both arms to control the steering wheel. To achieve this, the driver requires to have sufficient strength and mobility in their shoulder.
- It is the responsibility of the driver to ensure that they are in control of the vehicle at all times. They should be able to demonstrate this if stopped by the police.
- Drivers should check with their physiotherapist, surgeon and vehicle insurance policy before returning to drive after surgery.
- Drivers must not drive under the influence of narcotic medications or within a minimum of 24 hours after an anaesthetic.
In Summary
- You are NOT allowed to drive one handed
- There is no precise time after surgery when you can return to driving, it varies from person to person. However, the recommended amount of time that your arm should
be in a sling following surgery is the MINIMUM time before considering a return to driving - You can return to driving when you are capable of moving your shoulder without assistance and are capable of driving safely and reacting appropriately in an
emergency situation - Although it is not essential it may be wise to discuss your return to driving with your insurance company
More information about the estimated time before returning to drive following a specific procedure can be found in the respective rehabilitation protocol section for each procedure
Wound care
A plaster will be placed over the site of the injection. Please keep this clean and dry for 48 hours, after which you may remove the plaster and shower.
The wound is covered with a splash proof dressing. In the case of key hole surgery generally there are no stitches. In cases of open surgery there are dissolvable sutures which do not need to be removed.
We close all wounds with dissolving stitches and the knots are all buried under the skin, so no stitches need to be removed.
The shoulder surgery wounds are generally very small and heal in a cosmetically pleasing way. Over the wounds are placed paper stitches: Steri-strips to de-tension the wound and then splash proof dressings over them.
It is important to note that we say splash proof not water proof.
Usually, you can have a shower at 3 days post-surgery leaving the dressings intact, and trying not to get them wet.
At ten days the wounds should all be healed; the plasters may come off and you may shower normally again (within the parameters of the allowed shoulder movement from your rehab protocol). It is often best to leave the steri-strips on until they fall off naturally or until you come for a review in clinic.